Ureteral Stricture
What is Urethral Stricture?
Urethral stricture is a condition that occurs when the urethra (the urinary channel) abnormally narrows, obstructing the flow of urine. It is more common in men and may develop due to various causes. If left untreated, it can lead to serious kidney and bladder problems.
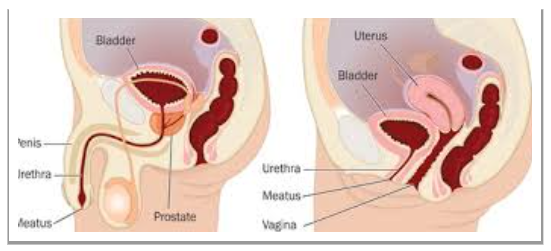
What Should Normal Urethral Anatomy Be Like?
The urethra is a tube-shaped channel that allows urine to pass from the bladder to the outside of the body. In men, it is approximately 20 cm long, while in women it is about 4 cm.
✔ The male urethra is divided into three main sections:
Anterior urethra (penile urethra): Has a more flexible structure.
Posterior urethra (membranous and prostatic urethra): Has a more rigid and fixed structure.
Bulbar urethra: The region where strictures most commonly develop.
✔ Since the female urethra is shorter, strictures are rarely seen.
Urethral stricture can occur in any part of the urethra and may hinder urine flow, significantly affecting the patient’s quality of life.
What Are the Causes of Urethral Stricture?
Urethral stricture can develop due to many different reasons. The most common causes include:
A) Traumatic Causes
✔ Pelvic Trauma: Traffic accidents, falls, or direct blows to the perineal region.
✔ After Urethral Catheterization or Endoscopy: Long-term catheter use, repeated cystoscopies.
✔ Trauma During Sexual Intercourse: Penile fracture or injury due to forced manipulation.
B) Infections
✔ Sexually Transmitted Infections (STIs): Especially gonorrhea and chlamydia.
✔ Urethritis (Inflammation of the Urethra): Chronic infections may lead to stricture formation.
C) After Surgical Interventions
✔ Prostate Surgeries: Urethral stricture may develop after TUR-P or radical prostatectomy.
✔ Hypospadias Repairs: Stricture may occur following correction of congenital urethral anomalies.
D) Congenital Causes
✔ Urethral Valves: Male infants may be born with an obstruction in the urethra.
E) Inflammatory and Autoimmune Diseases
✔ Lichen Sclerosus (Balanitis Xerotica Obliterans – BXO): A skin disease that causes scar tissue formation in the urethral mucosa.
What Are the Symptoms of Urethral Stricture?
The symptoms of urethral stricture may vary depending on the severity of the condition and the length of the narrowing:
✔ Difficulty urinating (the most common symptom)
✔ Decreased urine flow rate
✔ Split or intermittent urinary stream
✔ Post-void dribbling and feeling of incomplete bladder emptying
✔ Increased susceptibility to urinary tract infections
✔ Formation of bladder stones
✔ Complete obstruction (an emergency condition – inability to urinate and bladder distension, known as acute urinary retention)
If left untreated for a long time:
Kidney failure may develop.
The bladder may enlarge and lose its normal functions.
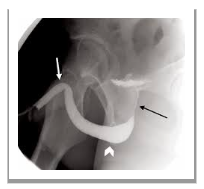
How Is Urethral Stricture Diagnosed?
✔ Infection:
One of the most important complications. Antibiotic-coated prostheses reduce the risk of infection.
If infection develops, the prosthesis may need to be removed.
✔ Mechanical Failure of the Prosthesis:
In inflatable prostheses, mechanical malfunctions may rarely occur.
In newer-generation prostheses, durability ranges between 10–15 years.
✔ Pain and Swelling:
Mild pain may occur during the first 1–2 weeks after surgery.
Painkillers and cold compresses can be applied.
How Do We Treat Urethral Stricture?
The treatment of urethral stricture depends on the length and location of the narrowing, as well as the patient’s overall health condition.
A) Temporary Solutions
✔ Urethral Dilatation (Widening)
The urethra is dilated using a balloon or bougie.
This is a temporary solution, and recurrence of the stricture is common.
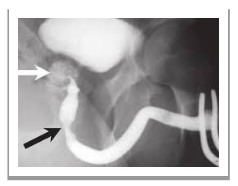
✔ Internal Urethrotomy (DVIU – Direct Visual Internal Urethrotomy)
The stricture is cut open endoscopically.
May be effective in short strictures (<1 cm), but the recurrence rate is high.
B) Permanent Solutions – Surgical Methods
✔ Urethral Reconstruction (Urethroplasty)
Considered the gold standard treatment method.
The narrowed segment is completely excised, and the urethra is reconstructed.
Types of Urethroplasty:
Primary Anastomotic Urethroplasty:
For short strictures (1–2 cm), the narrowed segment is excised and the ends are reconnected.Graft Urethroplasty:
For longer strictures, the urethra is reconstructed using a graft, often from buccal mucosa (oral lining).Pedicled Flap Urethroplasty:
An alternative surgical technique, used in severe cases.
✔ Urethral Stent Placement
Provides temporary relief in very elderly patients or those unfit for surgery.
When Should Open Surgery (Urethroplasty) Be Performed in Urethral Stricture?
The treatment method for urethral stricture is determined based on the length and location of the narrowing, the risk of recurrence, and the patient’s overall health condition. Open surgery (urethroplasty) is the most permanent treatment method and is preferred in the following situations:
✔ Strictures longer than 2 cm
✔ Recurrent strictures after endoscopic treatment
✔ Patients with severe scarring and fibrosis
✔ Patients with complete obstruction
✔ Penile urethral strictures
✔ Advanced strictures developed after trauma
In such cases, open surgery (urethroplasty) is the best option and provides a permanent solution.
If you provide detailed information about the patient’s condition, we can discuss the most appropriate treatment method for the specific case.
When Is Oral Tissue Used in Urethral Stricture Cases?
In open urethroplasty procedures, tissue taken from the mouth (usually buccal mucosa, i.e., the inner lining of the mouth) is preferred as an option that provides suitable tissue for urethral healing. Harvesting tissue from the oral cavity is especially used in cases where the urethra faces narrowing, stricture, or obstruction. The use of oral mucosa is common in the following situations:
Urethral strictures
When there is insufficient local tissue
When Other Tissue Sources Are Inadequate: If grafts taken from the groin or other body areas are insufficient, oral mucosa can serve as a good alternative.
Particularly in long-standing and extensive strictures, the use of buccal mucosa provides better healing and functional outcomes.
The use of buccal mucosa offers patients less pain and a lower risk of complications, while also supporting both functional and aesthetic recovery of the urethra in the long term.
What Should Be Considered After Urethral Stricture Surgery?
✔ Regular follow-up visits are required during the first 3–6 months after treatment.
✔ Adequate water intake is important to help prevent urinary tract infections.
✔ Early intervention is essential in cases of recurrent strictures.
Conclusion
✔ If not treated in a timely and appropriate manner, urethral stricture can lead to serious health problems.
✔ Endoscopic methods are effective in short strictures, while urethroplasty is the most effective treatment option for long or recurrent strictures.
✔ Early diagnosis and regular follow-up improve patients’ quality of life and help prevent serious complications such as kidney failure.
If you or a loved one has a specific condition related to urethral stricture, please contact us for more detailed information.
Mesajınızı İletin