Artificial Bladder
What Is an Artificial Bladder (Neobladder)?
An artificial bladder, or neobladder, is a surgically created urinary reservoir made from the patient’s own body tissue when the natural bladder must be removed due to various health conditions. It is most commonly performed in cases such as bladder cancer.
This surgical procedure is carried out to improve the patient’s quality of life and to help maintain urinary function as naturally as possible.
In Which Situations Is a Neobladder (Artificial Bladder) Performed?
Bladder Cancer: The most common reason for bladder removal. In such cases, the natural bladder is surgically removed and replaced with a neobladder.
Neural Tube or Spinal Cord Disorders: Conditions such as spinal cord injuries and other nervous system problems may affect urinary function. In these cases, a neobladder can be a solution.
Chronic Bladder Disorders: In certain chronic conditions that significantly reduce bladder capacity or impair its function, bladder replacement may be necessary.
Is a Neobladder Suitable for Every Patient?
A neobladder (artificial bladder) is not an appropriate option for every patient. The procedure depends on many factors, including the patient’s overall health, surgical eligibility, and lifestyle.
Patients Suitable for a Neobladder:
Those in Good General Health
Patients without serious systemic diseases such as heart, lung, or kidney disorders.Patients Whose Urethra Can Be Preserved
If the urethra is not affected by cancer and can be safely preserved, a neobladder may be performed.Patients with Suitable Bowel Condition
Not recommended for patients with a history of severe bowel diseases (such as Crohn’s disease or ulcerative colitis).Patients Who Can Learn to Void
Since a neobladder does not function exactly like a natural bladder with muscles and nerves, patients must learn how to urinate.
It is suitable for those who can use their abdominal muscles to empty urine.
Who Should Not Receive a Neobladder?
Patients in Poor General Health
Those with heart failure, severe lung disease, or advanced kidney failure.Patients Requiring Urethral Removal
If the cancer has invaded the urethra or if the urethra must be removed due to a tumor, a neobladder cannot be performed.Patients with Bowel Diseases
Inflammatory bowel diseases (such as Crohn’s disease or ulcerative colitis) make the bowel tissue unsuitable and the procedure risky.Patients Unable to Learn or Control Urination
Individuals with neurological disorders (such as spinal cord injury or multiple sclerosis) may not be able to control urination.
Elderly patients or those with impaired cognitive functions may also be unable to manage this process.
Although this procedure is relatively simple and safe from a technical standpoint, it is the most commonly used form of urinary diversion.
When choosing this type of urinary diversion, you should be aware that adapting to life with a stoma requires time and effort. Your healthcare team will help you adjust your lifestyle and adapt to the changes (such as altered body appearance, sports and hobbies, travel, etc.).
Are There Alternatives to a Neobladder?
If a neobladder is not suitable, other urinary diversion methods may be considered:
Ileal Conduit: Urine is diverted through a stoma (an opening in the abdominal wall).
Continent Urostomy (Indiana Pouch): An internal urine reservoir that is emptied using a catheter.
In conclusion, a neobladder may not be suitable for every patient and should be evaluated on an individual basis.
Would you like me to prepare a special assessment for your case or for a patient’s condition?
How Should the Preparation Process for a Neobladder Be?
Diagnosis and Evaluation:
Doctors may perform ultrasonography, cystoscopy, MRI, and CT scans to assess the condition of the urinary tract.
Counseling:
Psychological and physical counseling provides patients with information about the pros and cons of surgery, the recovery process, and life afterward.
Dietary Changes:
Before surgery, patients are usually advised to stop consuming alcohol and tobacco and to follow a light diet for preparation.
How Is a Neobladder Constructed?
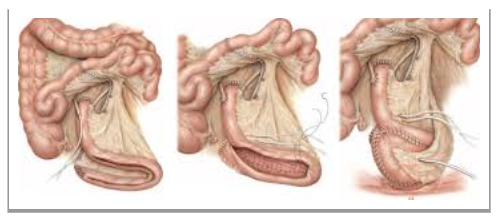
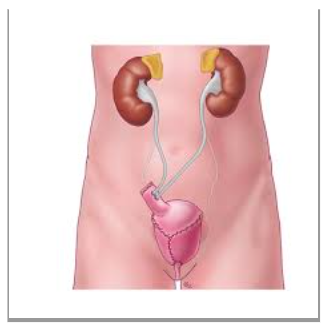
A 40–60 cm segment of the small intestine (ileum) is removed to be used as a substitute for the bladder. The remaining intestine is reconnected to the digestive system. The removed segment is flattened and then folded into a spherical or U-shape to create a pouch capable of storing urine.
The ureters (urinary ducts) are connected to the neobladder, allowing urine to flow from the kidneys into this new storage reservoir. When the neobladder is connected to the urethra, the patient can pass urine naturally by using their muscles. However, some patients may experience incontinence or difficulty emptying the bladder.
What Should Be Considered During the Recovery Process After Surgery?
Early Recovery Phase:
Observation: The first few days are spent in intensive care or in a closely monitored hospital unit.
Catheter Use: Urine may be drained through a catheter until the new bladder has fully healed.
Pain Management: Postoperative pain is managed with painkillers prescribed and supervised by the doctor.
Active Recovery:
Diet and Fluid Intake: Adjusting diet and ensuring adequate fluid intake are important, as sufficient hydration helps the urinary system function properly.
Gradual Physical Rehabilitation: Gentle physical activity supports recovery.
Bladder Training: Patients learn how to recognize signals when the bladder is full and how to use muscles effectively to maintain control.
What Should Be Considered in the Long Term with a Neobladder?
Regular Medical Check-Ups: Regular doctor visits are necessary to monitor healthy function and detect potential problems early.
Dietary Recommendations: Since kidney function may be affected, a diet low in protein and sodium may be advised.
Activity Level: Light regular exercise is recommended to maintain fitness and keep the intestines healthy.
Psychological Support: Counseling may help patients adjust emotionally and mentally.
Functional Management: For problems such as urinary incontinence or difficulty voiding, physical therapy and, when necessary, catheterization may be required.
What Complications Can Occur with a Neobladder?
Since neobladder (artificial bladder) surgery is a major surgical procedure, various short- and long-term complications may occur.
Early Complications (First Weeks After Surgery)
a) Surgical Complications
Bleeding
Anastomotic Leak (Urine Leakage): Urine may leak from the sites where the neobladder is connected to the ureters or urethra. This is usually managed with drainage, but in severe cases, reoperation may be necessary.
Bowel Problems: Intestinal obstruction (ileus) may occur, and if it does not resolve within a few days, surgical intervention may be required. Leakage at the intestinal suture sites can also occur, leading to serious infections.
b) Infections
Intermediate and Long-Term Complications
a) Functional Problems
Urinary Incontinence:
Daytime urinary control generally improves within a few months, but some patients may experience nighttime leakage. Kegel exercises are recommended to strengthen pelvic floor muscles.Difficulty Voiding:
Because the neobladder is not controlled by nerves, patients must learn to use abdominal muscles to urinate. Some patients may not fully empty their bladder and may need catheterization (draining urine with a catheter).
b) Metabolic Problems
Metabolic Acidosis:
When the bowel segment comes into contact with urine, bicarbonate loss can occur, leading to an acidic environment in the body. This may cause fatigue and shortness of breath. It can be corrected with sodium bicarbonate supplements.Kidney Dysfunction:
Over time, reflux of urine back into the kidneys (vesicoureteral reflux) may impair kidney function.
c) Stone and Mucus Formation
Stone Formation in the Neobladder:
Because the neobladder is made from intestinal tissue, stones may form inside it. Drinking plenty of water and regularly emptying the bladder can help prevent this.Mucus Production:
The intestinal segment continues to produce mucus, which can accumulate inside the bladder. Regular urination and, in some cases, bladder irrigation may be necessary.
Rare but Serious Complications
Fistula Formation: Abnormal connections may develop between the neobladder and the bowel, skin, or vagina.
Neobladder Stricture (Narrowing): Narrowing at the urethral connection site can occur, making urination difficult. Dilation or surgical intervention may be required.
Cancer Risk: After many years, there is a small risk of cancer developing in the bowel tissue used for the neobladder. Regular follow-up is essential.
Will I Be Able to Urinate Normally After a Neobladder?
With a neobladder, patients can largely return to normal life. However, since the new bladder does not have nerve connections, patients usually urinate by using their abdominal muscles. Some patients may need to empty urine with a catheter, and problems such as infections or stones may occur.
Patients may also need training on how to control and empty urine effectively.
Conclusion
Neobladder surgeries, due to their complexity and potential risks, require thorough evaluation. However, with modern medical technology and continuous treatment processes, patients experience a significant improvement in quality of life after surgery.
The medical team recommends that patients undergo a detailed preoperative consultation, during which the benefits, potential risks, and possible outcomes of the surgery are carefully explained.
An individualized treatment plan should always be created, tailored to each patient’s specific needs and life goals.
Mesajınızı İletin